About Joint Replacement
Your Treatment Options
Hip and Knee Pain
Topics
- Understanding the Causes of Joint Pain
- Treatment Options
- What Joint Replacement Surgery Involves
- Realistic Expectations After Joint Replacement

Did you know?
- More than 300,000 knee replacements are performed each year in the US.1
- More than 300,000 hip replacements are performed in the United States each year.2
Most Common Types of Arthritis
- Osteoarthritis
- Rheumatoid Arthritis
- Post-traumatic Arthritis
- Avascular Necrosis
- Paget’s Disease
Did you know?
Nearly 21 million Americans suffer from osteoarthritis, a degenerative joint disease that is a leading cause of joint replacement surgery.
Source: www.arthritis.org
OA Symptoms
- May develop suddenly or very slowly
- Arthritis can cause pain and stiffness
- Some types of arthritis may cause swelling
- Simple tasks may be difficult to do
Rheumatoid Arthritis, Post-traumatic Arthritis, Avascular Necrosis, Paget’s Disease
- Rheumatoid Arthritis – Membranes or tissues lining the joint become inflamed
- Post-traumatic Arthritis – Irregularities lead to more wear on the joint
- Avascular Necrosis – Bone may collapse and damage the cartilage
- Paget’s Disease – The density and the shape of the bone change
Did you know?
Rheumatoid arthritis, the most crippling form of arthritis, affects approximately 2.1 million Americans and two to three times more women than men. Further, the average onset for rheumatoid arthritis is between the ages of 20 and 45 years old.Source: CDC
Joint Degeneration
Pain from arthritis and joint degeneration can:
- Be constant
- Come and go
- Occur with movement
- Occur after a period of motionlessness
- Be located in one spot
- Be located in many parts of the body
- Be worse during certain times of the day
- Be worse after certain activities
Preparing for Your Doctor’s Visit
The Orthopaedic Evaluation
- A thorough medical history
- A physical examination
- X-Rays
- Additional tests, as needed
Medical History
A thorough medical history includes:
- A list of all medications you are currently taking
- Information on prior surgeries and/or treatments
- Prior diagnoses
- Family history
The information that the surgeon gathers during the medical history usually suggests the possibility of several different diagnoses.
The physical examination enables your surgeon to evaluate important aspects of your joints, including:
- Size and length
- Strength
- Range of motion
- Swelling
- Reflexes
- Skin condition
X-Ray Evaluation
X-Rays help show how much joint damage or deformity exists. An abnormal X-ray may reveal:
- Narrowing of the joint space
- Cysts in the bone
- Spurs on the edge of the bone
- Areas of bony thickening called sclerosis
- Deformity or incorrect alignment
Additional Diagnostic Tests
Occasionally, additional tests may be needed to confirm the diagnosis. These may include:
- Blood tests
- Urine analysis
- Analysis of joint fluid
- Magnetic Resonance Imaging (MRI)
- Bone scan
Treatment Options
- Medication
- Physical therapy
- Arthroscopy – cleaning the joint
- Joint fluid supplements (injections that provide temporary pain relief)
- Partial joint replacement
- Total joint replacement
Medications
- Aspirin-free pain relievers–acetaminophen
- Nonsteroidal anti-inflammatories (NSAIDs)
- Corticosteroids–injection/pill form
Physical Therapy
- Passive range-of-motion exercises may help:
– Reduce stiffness
– Keep joints flexible - Isometric exercises help build muscle strength
Arthroscopy
What is arthroscopy?
Arthroscopy is a surgical procedure used to visualize, diagnose and treat problems inside a joint.
In an arthroscopic examination, an orthopaedic surgeon makes a small incision in the patient’s skin and then inserts pencil-sized instruments that contain a small lens and lighting system to magnify and illuminate the structures inside the joint.
Joint Fluid Supplements
Injections that provide temporary relief:
- For patients whose joint pain does not improve with medication or physical therapy, “joint grease” injections may provide temporary relief. The joint is injected with a joint fluid supplement that acts as a lubricant for the damaged joint.
- Joint injection schedules and duration of relief vary according to the treatment chosen and the individual patient. However, these injections do not cure the diseased knee, and joint replacement may be needed as the joint worsens with time.
Partial Joint Replacement
Partial joint replacement is a surgical procedure in which only the damaged or diseased surfaces of the joint are replaced, leaving much of the natural bone and soft tissue in place.
Total Joint Replacement
Total joint replacement is a surgical procedure in which certain parts of an arthritic or damaged joint are removed and replaced with a plastic or metal device or an artificial joint. The artificial joint is designed to move just like a healthy joint.
Joint Replacement
Joint replacement is a treatment option when pain:
- Is severe
- Interferes with daily activities
- Interferes with work
Joint replacement is a decision that should include:
- You
- Your primary care provider
- Your orthopaedic surgeon
Did you know?
Total joint replacements of the hip and knee have been performed since the 1960s. Today, these procedures have been found to result in significant restoration of function and reduction of pain in 90% to 95% of patients.
Source: National Development Conference, National Institutes of Health, December 2003
Joint Replacement Preoperative
Preparing for a joint replacement procedure begins weeks before the actual day of surgery.
In general, patients may need:
- Routine blood tests
- Urinalysis
- Physical examination
- Exercise
- Quit smoking
- Stop certain medications
- Donate blood
Joint Replacement Preoperative
- A general physical examination
- Dental procedures
- Skin condition
- Smoking
- Weight
- Medications
Your Hip Joint
A joint is formed by the ends of 2 or more bones. The hip must bear the full force of your weight and consists of two main parts:
- A ball (femoral head) at the top of your thigh bone (femur)
- A rounded socket (acetabulum) in your pelvis


What Causes Hip Joint Pain?
One of the most common causes of joint pain is arthritis. The most common types of arthritis are:
- Osteoarthritis (OA)
- Rheumatoid Arthritis (RA)
- Post-traumatic Arthritis
- Avascular Necrosis
Hip Surgery
May be suitable for patients who:
- Have a painful, disabling joint disease of the hip resulting from a severe form of arthritis
- Are not likely to achieve satisfactory results from less invasive procedures, medication, physical therapy, or joint fluid supplements
- Have bone stock that is of poor quality or inadequate for other reconstructive techniques
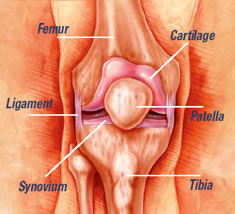
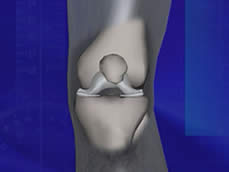
Your Knee Joint
Femur – thigh bone
Cartilage – tissue between bones that provides cushioning
Patella – knee cap
Tibia – shin bone
Synovium – tissue that provides lubricating fluid to joint
Ligament – flexible tissue that holds knee joint together
What Causes Knee Joint Pain?
One of the most common causes of joint pain is arthritis. The most common types of arthritis are:
- Osteoarthritis (OA)
- Rheumatoid Arthritis (RA)
- Post-traumatic Arthritis
Knee Surgery
May be suitable for patients who:
- Have a painful, disabling joint disease of the knee resulting from a severe form of arthritis
- Are not likely to achieve satisfactory results from less invasive procedures, medication, physical therapy, or joint fluid supplements
- Have bone stock that is of poor quality or inadequate for other reconstructive techniques

Total Knee Joint Replacement
- End surface of femur replaced with metal
- End surface of tibia replaced with metal
- Plastic liner is inserted between femur and tibia to reduce wear
- Patella is resurfaced with plastic
Recovery
Every individual is different and every treatment plan is different. The length of hospital stay after joint replacement varies and depends on many factors including age and physical ability.
Estimated Recovery Schedule
- In-hospital Recovery: 2 – 5 days
- Significant Functional Improvement: 6 weeks – 3 months
- Maximal Improvement: 6 – 12 months
Recovery — Rehabilitation
Following joint replacement the physical therapist begins an exercise program to be performed in bed and in the therapy department. The physical therapist or another member of the staff works with the patient to help the patient:
- Regain muscle strength
- Increase range of motion
When will I be able to go back to a normal daily routine?
This is a decision only you and your surgeon can make. Every patient’s experience is different.
However, there are some general guidelines your doctor may give you:
- You’ll practice stair — climbing in the hospital and should be able to do this by the time you leave
- You should have no restrictions on leaving your home as long as your safety and comfort are assured. Just don’t tire yourself out; a good balance of exercise, rest, and relaxation is best for helping your body heal and gain strength
- When to resume driving a car, going to work, and/or participating in sports activities are all highly individualized decisions. Be sure to follow your doctor’s or orthopaedic surgeon’s advice and recommendations
After Surgery — Limitations
For approximately 12 weeks after surgery certain limitations are placed on your activities. When fully recovered, most patients can return to work. However, some types of work may not be advisable for individuals with a joint replacement. These types of work include:
- Construction work
- Certain types of carpentry
- Occupations that involve repeated high climbing
Athletic activities that place excessive stress on the joint replacement will need to be avoided. Examples of these activities include:
- Skiing (snow or water)
- Basketball
- Baseball
- Contact sports
- Running
- Frequent jumping
Realistic Expectations
Physical Activities
After joint replacement, acceptable physical activities should:
- Not cause pain — including pain felt later
- Not jar the joint — running and jumping should be avoided
- Not place the joint in the extremes of its range of motion
- Be pleasurable
Longevity of Joint Replacement
It is impossible to predict in individual cases how long a joint replacement will last. Many factors determine the outcome including:
- Age
- Weight
- Activity level
- Bone strength
